For millions of people worldwide, blood thinners play a crucial role in preventing life-threatening health emergencies. However, while these medications can save lives, they also carry significant risks that require careful monitoring and management. Experts are increasingly asking an important question: Blood thinners are among the top contributors to medication-related complications—can these risks be reduced?
A Lifeline With Challenges
At 65, Larry Bordeaux has relied on blood thinners since 2010, after he began developing dangerous blood clots following surgery. He believes the medication saved his life. Whenever he temporarily stops taking the drugs before undergoing certain medical procedures, he quickly develops clots again.
Despite their benefits, Bordeaux understands the downside of these medications. Blood thinners increase the chances of severe and uncontrollable bleeding. Over the years, he has faced several complications, including a serious hematoma, where blood collects outside blood vessels, and episodes of gastrointestinal bleeding.
Bordeaux, who lives in Havelock, North Carolina, warns that even minor injuries can become dangerous. He now works with the National Blood Clot Alliance, a nonprofit organization dedicated to reducing clot-related deaths and minimizing complications associated with blood-thinning medications.
Millions Rely on Anticoagulants
Bordeaux is not alone. More than 8 million Americans take blood thinners, medically known as anticoagulants. Many patients begin using them after developing clots following surgery, while others rely on them to manage atrial fibrillation, a common age-related heart rhythm disorder that increases the likelihood of clot formation.
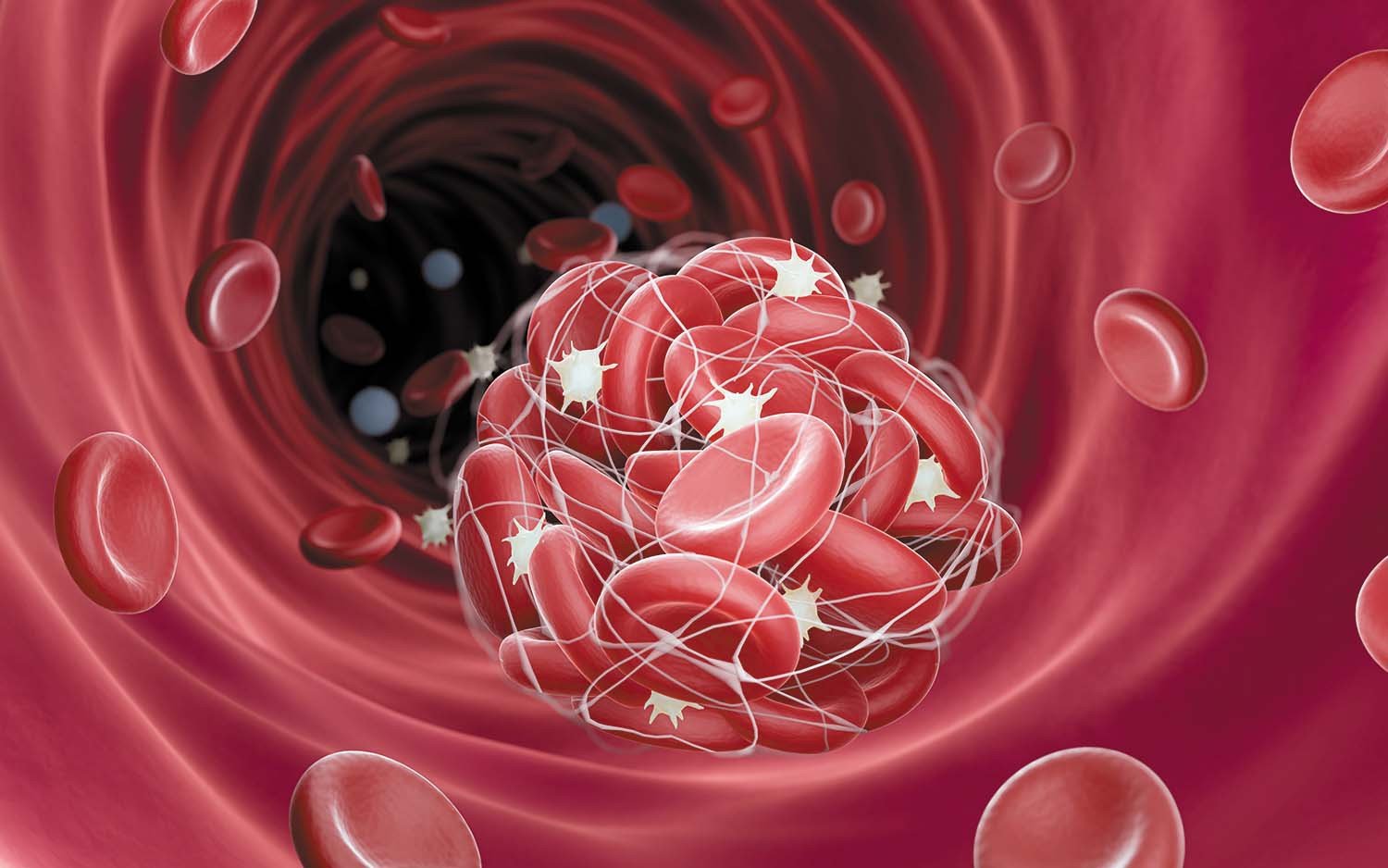
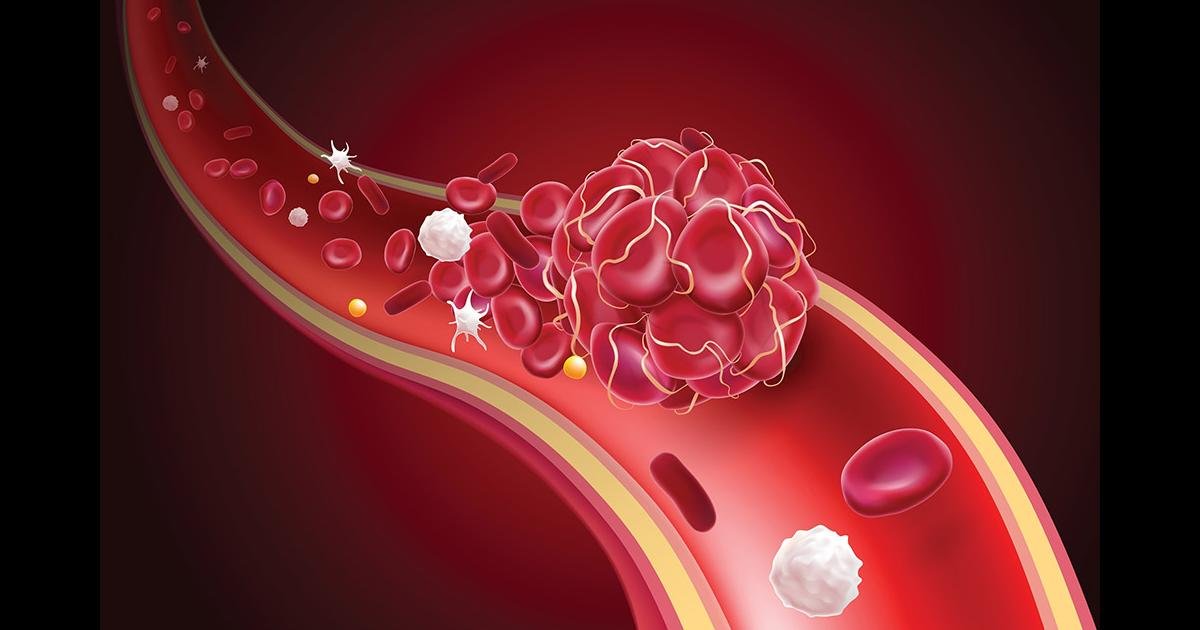
Blood clotting is a natural and necessary bodily process that helps stop bleeding after injury. However, excessive clotting can block blood vessels, leading to embolisms, strokes, and heart attacks. Blood thinners reduce these risks by interfering with clot formation, but they can also trigger serious bleeding events.
These complications place a heavy burden on the healthcare system. Research published in the American Journal of Medicine estimates that bleeding incidents linked to blood thinners send hundreds of thousands of older adults to hospitals each year, costing over $2.5 billion annually.
Balancing Protection and Risk
Cardiovascular specialists explain that blood thinners significantly reduce the risk of ischemic strokes caused by blocked blood flow. However, they can slightly increase the risk of hemorrhagic strokes, which result from bleeding in the brain.
Experts also warn that bleeding complications often occur in the stomach or digestive tract. In severe cases, patients may require blood transfusions or emergency treatment. Other possible side effects include prolonged bleeding from cuts, persistent nosebleeds, blood in urine, and, in rare cases, bleeding in the lungs or brain.
Medical professionals emphasize that patients and their families are often unaware of these risks. Advocates argue that bleeding incidents should not be dismissed as unavoidable complications, as research suggests nearly half of such adverse events may be preventable.
A Shift Toward Modern Blood Thinners
For decades, warfarin was the primary anticoagulant prescribed to patients. Although effective, it required frequent blood tests to adjust dosage levels because its effects varied widely between individuals.
In 2010, a newer group of medications known as direct oral anticoagulants (DOACs) was introduced. These include drugs such as apixaban, dabigatran, edoxaban, and rivaroxaban. Clinical trials showed that these medications were generally safer and more predictable than warfarin.
However, real-world data reveals that bleeding risks remain significant. Each year, roughly 300,000 Americans using anticoagulants still require emergency treatment for bleeding complications. Experts believe that reduced monitoring requirements may sometimes lead to insufficient oversight, increasing the chances of medication misuse or extended use beyond recommended periods.
Medication Interactions Increase Danger
Another major concern involves combining blood thinners with other medications. For example, pairing anticoagulants with antiplatelet drugs—often prescribed after heart attacks—can sharply raise bleeding risk. Studies suggest that a considerable portion of patients take both types of medications without clear medical necessity.
Similarly, over-the-counter drugs like aspirin can act as additional blood thinners. Research shows that nearly one-third of patients taking anticoagulants for certain conditions also regularly use aspirin, often without proper guidance, further increasing the risk of serious bleeding events.
Doctors also stress the importance of proper dosing. Factors such as age, kidney function, weight changes, and fall risk can all influence how a patient should use blood thinners. Incorrect dosing or failure to adjust medication over time can significantly increase the likelihood of severe complications.
Improving Safety Through Smarter Monitoring
Healthcare professionals believe that better training and specialized care could reduce dosing errors. Some experts argue that anticoagulants should not be prescribed if the patient’s bleeding risk outweighs potential benefits. However, doctors must carefully weigh these decisions, as avoiding blood thinners entirely can increase the risk of stroke.
Hospitals are increasingly turning to advanced predictive technologies to improve patient safety. Artificial intelligence systems and electronic health record tools can help identify patients who require dosage adjustments or specialist consultations. These systems can also flag dangerous drug interactions or health changes that might increase bleeding risks.
Future Treatments Offer Hope
Researchers are also exploring new treatment strategies that could reduce reliance on long-term blood thinner use. One promising approach is cardiac ablation, a procedure that corrects irregular heart rhythms and may allow some patients with atrial fibrillation to stop anticoagulant therapy altogether.
Additionally, scientists are studying a new class of medications called Factor XIa inhibitors. These drugs target specific proteins involved in clot formation and may reduce bleeding risks while maintaining effectiveness in preventing dangerous clots.
Moving Toward Safer Care
Medical experts agree that improving blood thinner management could prevent thousands of emergency hospital visits each year. Better patient education, careful medication monitoring, and advancements in treatment could significantly reduce complications.
While blood thinners remain essential for preventing strokes and deadly clots, healthcare professionals continue searching for ways to make these life-saving medications safer. As research advances, the hope is that patients like Larry Bordeaux can continue benefiting from anticoagulants with fewer risks and better overall protection.